Healthcare staffing has become both a lifeline and a legal minefield in 2025. Hospitals and healthcare systems rely heavily on temporary healthcare staffing, travel clinicians, and per-diem healthcare staffing clinicians to cover workforce shortages. But with this reliance comes heightened scrutiny: compliance with OSHA standards, Centers for Medicare & Medicaid Services (CMS) guidelines, and state-specific licensure rules is mandatory, and mistakes can be costly for any healthcare staffing agency or provider.
Hospitals must ensure that their staffing partners are not only delivering qualified talent but also adhering to federal and state regulations. In this guide, we’ll examine the compliance challenges that hospitals face, explore best practices for vetting staffing vendors, and outline strategies for protecting patient safety while minimizing organizational risk in today’s evolving healthcare workforce solutions environment.
Major Healthcare Staffing Compliance Challenges and Credentialing Risks
Compliance issues in healthcare staffing can quickly escalate into legal liabilities, fines, or threats to patient safety. The most pressing healthcare staffing challenges include:
- Credentialing and Licensure Verification
Every temporary clinician must hold an active license in the state they are practicing. Failing to verify licenses verification can result in regulatory violations and potential malpractice liability. Strong credentialing compliance protects both hospitals and staffing vendors. - OSHA and Workplace Safety Standards
Agencies and hospitals are both accountable for ensuring clinicians have completed required workplace safety training, including infection control and bloodborne pathogens. Poor adherence to OSHA healthcare compliance standards remains a major risk during staffing surges. - CMS Staffing Ratios and Patient Safety Regulations
CMS enforces staffing standards for hospitals that participate in Medicare and Medicaid. Failure to meet minimum nurse-to-patient ratios can jeopardize funding and accreditation. Monitoring CMS staffing ratios is now a core part of modern hospital staffing services. - Co-Employment Risks
Hospitals and staffing agencies must clearly define responsibilities to avoid “joint employer” liabilities related to pay, benefits, and workplace disputes. Mismanaged co-employment risk exposes hospitals to wage, hour, and compliance claims. - State-by-State Variations
Each state sets its own licensure, ratio, and overtime rules. A clinician eligible in New York may not meet requirements in California. Tracking these nuances is essential for any organization relying on medical staffing solutions.
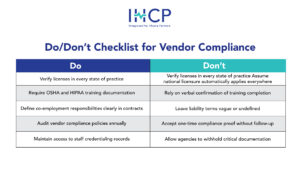
How to Vet a Healthcare Staffing Agency for Compliance and Vendor Risk
Hospitals cannot afford to take compliance claims at face value. Vetting vendors thoroughly ensures risks are minimized while improving resilience during surges in healthcare staffing trends.
Best Practices:
- Request Documentation: Ask for evidence of license verification processes, background checks, and credential audits, and clinician verification.
- Audit Vendor Policies: Review how agencies handle OSHA training, HIPAA compliance, and immunization record-keeping.
- Check Joint Commission Accreditation: The Joint Commission certifies staffing agencies that meet rigorous compliance criteria—an essential filter when choosing the best healthcare staffing agency partner.
- Demand Transparency: Hospitals should require real-time access to credentialing and staffing records to confirm vendor compliance audits.
Protecting Patient Safety Through CMS Staffing Ratios and Hospital Staffing Services
Improper staffing ratios directly impact patient outcomes. A landmark 2022 study published in Health Affairs found that for every additional patient added to a nurse’s workload, the likelihood of patient mortality increased by 7%. This makes compliant hospital staffing services critical for patient safety.
CMS & OSHA Guidelines
- CMS (42 CFR §482.23): Requires hospitals to provide “adequate numbers of licensed registered nurses” for safe patient care.
- OSHA Standards: Require employers to ensure that working conditions—such as overtime scheduling and workload management—do not pose safety hazards.
Staffing agencies that specialize in emergency healthcare staffing or rapid response healthcare staffing can help facilities maintain safe ratios during surges. However, ultimate compliance responsibility still lies with the hospital.
Avoiding Co-Employment Risk in Healthcare Staffing Contracts
Co-employment is one of the most misunderstood risks in healthcare staffing compliance. If roles and responsibilities between hospital and staffing agency are not clearly defined, both parties may be considered “joint employers.”
Risks Include:
- Liability for wage and hour violations
- Responsibility for benefits and leave policies
- Exposure to workplace harassment or discrimination claims
Risk Mitigation Steps
- Clearly define who manages scheduling, supervision, and performance evaluations.
- Specify payroll and benefits responsibilities in contracts.
- Use indemnification clauses to limit liability exposure.
These practices are now standard across sophisticated healthcare consulting firms and healthcare recruitment consulting partners.
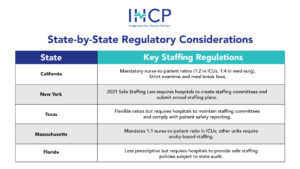
State-by-State Healthcare Staffing Compliance and OSHA Requirements
Healthcare staffing is not a one-size-fits-all process. State regulations vary widely, particularly regarding licensure, staffing ratios, and overtime laws. This complexity is why many providers work with experienced executive placement firms and compliance-focused staffing partners.
Example Legislative Excerpts:
- California Health & Safety Code §1276.4: “Hospitals shall maintain a nurse-to-patient ratio sufficient to ensure patient safety.”
- OSHA 29 CFR §1910.1030: Mandates training for all staff at risk of exposure to bloodborne pathogens.
Hospitals must track not only federal requirements but also each state’s shifting standards, a growing challenge amid nationwide staffing shortages.
Conclusion: Reducing Liability With Compliant Healthcare Workforce Solutions
Healthcare staffing compliance is more than a box-checking exercise, it’s about protecting patients, minimizing legal risk, and maintaining accreditation. From state-specific licensure rules to OSHA and CMS staffing mandates, hospitals must ensure their staffing partners meet every requirement.
The stakes are high: missteps can lead to regulatory fines, funding loss, or compromised patient safety. By thoroughly vetting vendors, maintaining access to documentation, and monitoring ratios, hospitals can turn staffing from a risk into a strategic advantage.
In 2025, strong healthcare staffing compliance practices are no longer optional—they’re a cornerstone of safe, sustainable care delivery.
FAQ: Healthcare Staffing Compliance, Credentialing & Vendor Verification
Q: What are common compliance challenges in staff surges?
A: The biggest challenges include rushed credentialing, missed background checks, and failure to verify state-specific licenses. Compliance risks rise when hospitals bypass standard onboarding to fill urgent needs in temporary healthcare staffing or emergency healthcare staffing situations.
Q: How can hospitals verify staffing partner compliance?
A: Hospitals should request real-time access to credentialing databases, require Joint Commission-accredited vendors, and audit staffing partners annually. Independent vendor compliance audits are also recommended.
Q: What documentation is required for temporary staff?
A: Required documents typically include: active state license, background check, immunization records, drug screening results, certifications (BLS, ACLS, etc.), OSHA safety training, and proof of work eligibility (I-9). Ensuring strong credentialing compliance avoids regulatory penalties.