The quality of patient care is deeply intertwined with the competency and confidence of healthcare staff. As medical systems grow more sophisticated and patient expectations continue to evolve, healthcare organizations must invest in continuous, structured medical training programs that equip staff with the knowledge, empathy, and adaptability necessary to deliver exceptional care.
This blog explores the relationship between healthcare staff training and patient outcomes, outlines strategies for developing robust healthcare training solutions, examines the role of technology, and discusses how to measure the true impact of training investments on healthcare quality.

Introduction: The Link Between Staff Training and Patient Outcomes in Healthcare
Healthcare is a people-driven industry, and the knowledge, skills, and behaviors of clinical and non-clinical staff directly impact patient experiences and health outcomes. Well-trained employees are more likely to recognize early warning signs of deterioration, follow protocols accurately, communicate effectively, and create a safe, reassuring environment for patients and families.
In this guide, we explore how targeted healthcare workforce development and clinical staff development improves both individual performance and systemic quality. Organizations that prioritize structured training not only reduce errors and improve compliance—but also see measurable gains in patient satisfaction, team morale, and operational efficiency.
Designing Comprehensive Healthcare Training Programs for Clinical Teams
Effective hospital staff training programs don’t happen by accident. They require thoughtful design, customization, and alignment with both organizational goals and frontline realities. A successful training program must bridge the gap between theory and practice.
1. Needs Assessment and Role-Based Planning
Before designing content, healthcare organizations should assess gaps in performance, knowledge, or compliance. This could be done through:
- Incident reports and patient feedback analysis.
- Compliance audit results.
- Staff surveys and manager interviews.
Each medical training program should be customized to the unique challenges of the role—whether it’s for nurses, administrative staff, lab technicians, or housekeeping teams.
2. Modular and Progressive Learning Paths
Instead of overwhelming employees with dense, one-size-fits-all sessions, structure learning paths that:
- Start with foundational knowledge.
- Progress to scenario-based or skills-focused modules.
- Include periodic refreshers and updates.
For example, a progressive path for nurses might include modules on wound care, medication reconciliation, and cultural competency—each building upon the last.
3. Compliance and Credentialing Integration
Training programs should be aligned with regulatory requirements (HIPAA, OSHA, CMS standards, etc.) and linked to ongoing credentialing needs. This ensures that staff remain compliant while also acquiring practical, job-specific skills.
Incorporating Technology into Medical Training Programs
Traditional in-person training has its place, but integrating modern technology can elevate learning experiences and make training more accessible, engaging, and scalable.
1. Learning Management Systems (LMS)
An LMS for healthcare training allows organizations to deliver consistent training content, track completion, and evaluate performance across departments. Features may include:
- Interactive modules and video-based lessons.
- Real-time quizzes and skill assessments.
- Dashboards for tracking compliance.
Cloud-based platforms allow staff to learn at their own pace, across shifts or facilities.
2. Simulation-Based Learning
Healthcare simulation training labs or virtual reality medical training scenarios provide immersive, hands-on experience without patient risk. Trainees can practice responding to code blue situations, inserting catheters, or managing aggressive patients in a controlled environment.
Benefits include:
- Improved confidence and muscle memory.
- Reduced anxiety in real-world situations.
- Safer onboarding of new hires.
3. Mobile Microlearning
Short, bite-sized training videos or interactive scenarios delivered via mobile devices are ideal for busy healthcare environments. Microlearning keeps content fresh and digestible while reinforcing key points through repetition.
Topics might include:
- Hand hygiene protocol.
- De-escalation techniques for patient aggression.
- Data entry tips in electronic health records.
4. AI-Powered Personalization
AI can tailor content delivery based on the learner’s past performance, role, and learning style. For example, if a clinician struggles with medication calculations, the system can provide targeted refreshers and supplemental exercises.
Measuring Training Effectiveness
Training programs should be evaluated not just by completion rates—but by their real-world impact on improving patient outcomes through training, safety, and employee performance. A data-driven approach ensures continuous improvement.
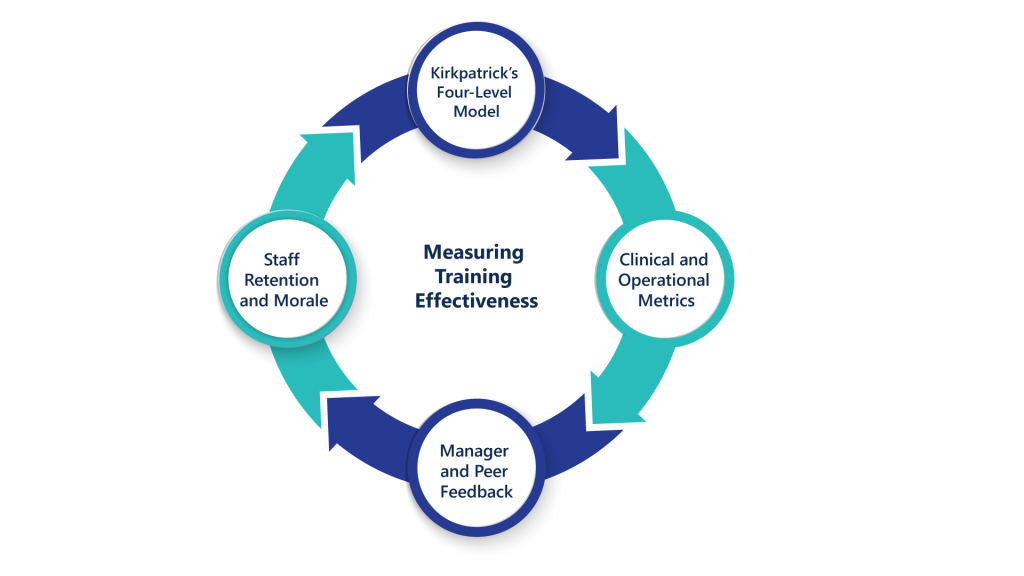
1. Kirkpatrick’s Four-Level Model
A widely used framework to evaluate training effectiveness:
- Reaction – Did employees find the training engaging and relevant?
- Learning – Did they acquire new knowledge or skills?
- Behavior – Are they applying the new skills on the job?
- Results – Is there measurable impact on patient outcomes, satisfaction, or efficiency?
Use surveys, quizzes, observations, and key performance indicators (KPIs) to gather insights at each level.
2. Clinical and Operational Metrics
Training success can be linked to tangible healthcare outcomes such as:
- Reduction in medication errors.
- Improved patient satisfaction (HCAHPS scores).
- Fewer staff injuries or OSHA incidents.
- Faster onboarding-to-productivity timelines.
Regularly compare these metrics before and after training rollouts.
3. Manager and Peer Feedback
Supervisors and colleagues offer valuable insights into behavior change and performance. Encourage structured feedback through 360-degree reviews, shadowing, or informal check-ins after training is completed.
4. Staff Retention and Morale
Employees who feel supported and continuously developed are more likely to stay. Effective training contributes to a culture of learning, belonging, and upward mobility—key drivers of long-term retention.
Conclusion: Investing in Continuous Healthcare Workforce Development
The most effective healthcare organizations understand that staff development is not a one-time event—it’s an ongoing commitment. By investing in comprehensive, technology-enabled, and personalized healthcare staff training, leaders can create a workforce that is confident, competent, and capable of delivering exceptional patient care.
In this guide, we’ve discussed how to design impactful training modules, integrate digital tools, and measure performance beyond surface-level metrics. When staff feel prepared, patients feel safe—and outcomes improve across the board.
Integrated HCP: Training Programs That Power Clinical Staff Performance
At Integrated HCP, we believe that great care begins with great people—and great people are made stronger through consistent, expert-led medical training programs. That’s why we help healthcare organizations build custom healthcare training solutions that drive both employee growth and patient safety.
Our training and talent solutions include:
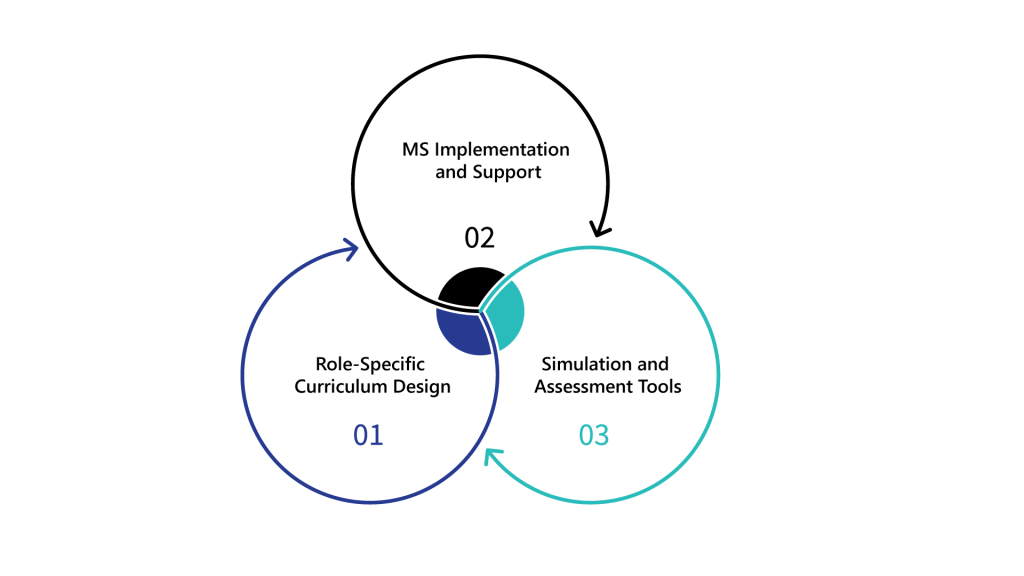
- Role-Specific Curriculum Design aligned with your care delivery model.
- LMS Implementation and Support for streamlined learning.
- Simulation and Assessment Tools that prepare staff for real-world challenges.
Let us help you enhance performance at every level—visit IHCP to explore training solutions that improve retention, compliance, and patient trust.